Why I Want More Than The Med Diet For My Patients
I want to begin here, because I have no interest in dismantling something that works. The Mediterranean Diet works, and the research supporting it is extensive, with olive oil, fish, vegetables, legumes, and whole grains forming a way of eating that correlates with lower rates of heart disease, diabetes, and cognitive decline across multiple populations studied over decades. When patients tell me they've been trying to eat Mediterranean, I tell them that's wonderful and to keep doing exactly that, because the dietary pattern itself has genuine merit and nothing I'm about to say changes that fundamental reality. The foods are good. The emphasis on plants and healthy fats makes physiological sense. The cultural tradition of eating slowly, with others, around a table, carries its own benefits that go beyond macronutrients.
What I need in my practice goes beyond a list of foods that epidemiologists have correlated with longevity in Southern European populations. When I sit across from a woman who has tried everything, who knows precisely what she "should" be eating and still finds herself unable to make it stick week after week, I need tools that help her understand what's actually happening in her body on a given Tuesday afternoon when the day has gone sideways and dinner feels impossible to navigate. I need a way to see patterns she cannot see herself, a method of tracking that teaches her something useful about her own eating rather than simply documenting her perceived failures. The Mediterranean Diet Score, whatever its merits for population research, was designed to study broad dietary patterns across thousands of people, which serves a different purpose than what I'm trying to accomplish with individual patients who need actionable, personalized feedback about their own nutrition. So I built something else.
What the Med score actually measures
The original Mediterranean Diet Score was developed for epidemiologists studying health outcomes across large populations, which means it uses median cutoffs in which the definition of adequate intake varies depending on who is in the study. What counts as sufficient fibre in one Greek population might be considered inadequate in a study of Italian villagers, and neither threshold necessarily applies to a professional woman in Toronto trying to determine whether her eating patterns are serving her well. For research purposes, this flexibility is justified because you're comparing individuals within the same study population to identify relative patterns and draw conclusions about associations with health outcomes. For a patient who wants consistent feedback week after week, a measuring stick that keeps changing its own calibration creates confusion rather than clarity, and she ends up feeling like the goalposts are moving even when her eating stays the same.
The scoring system also awards points for moderate alcohol consumption, which made historical sense when researchers were studying cultures where wine accompanies meals as a matter of course and abstinence was relatively rare. In practice, this creates real problems when I'm working with a patient who has decided, for whatever reason, to reduce or eliminate drinking, because she shouldn't feel punished for that choice, and a nutrition assessment built for her life shouldn't treat sobriety as a deficit. The score ignores timing entirely, treating calories consumed at breakfast identically to calories consumed at midnight despite substantial research on circadian biology showing that your body processes the same food differently at different times of day. It doesn't specifically measure protein intake, which matters enormously for muscle preservation during weight loss and for satiety after meals. It doesn't track hydration, even though thirst frequently masquerades as hunger and makes accurate appetite reading nearly impossible.
What I wanted to build
Since 2023, I have used the RxFood platform with every patient in my practice. Patients photograph their food rather than manually logging it, and the platform interprets those images and translates them into information my clinical team can act on: diet quality scores, nutrient balance, intake patterns over time. RxFood makes it easy to track food and easy to start understanding what matters in nutrition, which has been transformative for patients who previously found logging tedious or overwhelming. The platform has allowed me to see, in real time, what my patients are actually eating, how those patterns relate to their symptoms, which medications are working, and where gaps are forming.
What I've observed over these years of watching nutrition data flow through my practice is that the standard metrics don't capture what actually matters for the women I treat. I see patients hitting conventional targets while still feeling terrible. I see women whose "diet quality" looks fine on paper but whose eating patterns are setting them up for muscle loss, energy crashes, and medication side effects that could have been prevented. I see the gap between population-level recommendations and individual-level needs, and I've spent years thinking about how to close it.
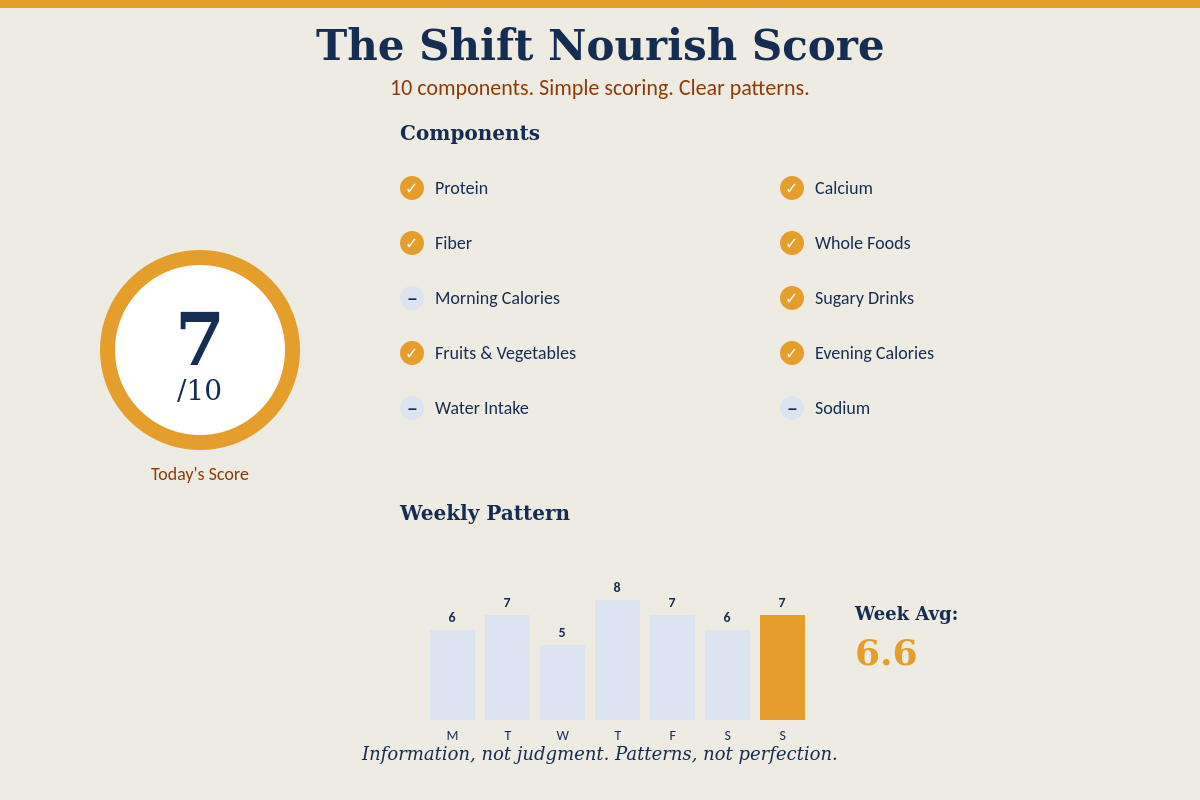
The Shift Nourish Score is what I built to address that gap. It launches this week and represents everything I've learned about what nutrition tracking should measure when the goal is appetite regulation rather than merely "eating better" in an abstract sense.
Why I chose these components
Protein matters because it protects muscle mass during weight loss and produces lasting satisfaction after meals, which means patients who hit their protein targets tend to feel genuinely full rather than fighting hunger all afternoon. Fibre matters because it feeds the gut bacteria involved in appetite signalling and stabilizes blood sugar, reducing the spikes and crashes that trigger urgent wanting and late-night pantry raids. Timing matters because your body processes the same food differently depending on time of day, with morning calories generally supporting better metabolic outcomes and late-night eating often disrupting sleep and next-day appetite. Hydration matters because even mild dehydration can produce sensations that feel identical to hunger, making it harder to read what your body actually needs.
I selected components that directly align with what I've observed in practice: patterns correlating with patients feeling regulated versus chaotic, and eating behaviours that predict success on medication versus those that predict struggle. They're the result of years of watching what actually happens when women try to change their eating in the context of comprehensive weight care.
Each component is scored as either zero or one, so you either met the threshold or you didn't, with no weighted averages, no complicated formulas, and no numbers requiring a calculator to interpret. I made this choice because I've watched too many patients get lost in optimization, adjusting and recalculating and tweaking until the tracking itself becomes another source of stress that crowds out everything else they're trying to accomplish. A compass tells you which direction you're facing without demanding that you calculate your precise longitude, and the Shift Nourish Score works the same way: quick orientation that tells you where you are, with enough specificity to be useful and enough simplicity to avoid overwhelm.
How the dashboard will work
In practice, patients will see their Nourish Score on a dashboard that updates based on the food they log through RxFood, which means they'll receive feedback on how their patterns are tracking without waiting for a monthly review or a scheduled appointment to determine whether they're on course. The score will appear as a simple number out of ten, and below it, the individual components will indicate which items the patient met and which she didn't. If someone scores a six, she will immediately see that she has met her protein and fibre targets but missed her morning calorie targets, hydration, and vegetable servings. That specificity matters because it transforms a vague sense of "I should eat better" into concrete information about what might be worth adjusting, and it does so in a way that makes clear she's doing some things well even on days when the overall score feels lower than she'd like.
The design philosophy behind the dashboard emphasizes information over judgment, which affects everything from the colour palette to the language we use. There are no red warning colours screaming about calories exceeded, no shaming language about going "over" or being "bad," because that kind of negative reinforcement triggers exactly the nervous system state where regulated eating becomes impossible, pushing patients toward the reactive mode where appetite signals scramble, and food decisions feel urgent and desperate. The interface presents facts with curiosity rather than criticism. Here's what you ate. Here's how it maps to the components we measure. Here's your score for the day and for the week. What you do with that information remains your choice, and the tool itself maintains neutrality because the last thing my patients need is another voice telling them they've failed.
Patients will be able to check the dashboard as often or as little as they want, and I'll encourage them to find a rhythm that feels useful rather than compulsive. Some will look daily while they're building new habits; others will check weekly to see patterns over time. The dashboard includes a weekly view that averages individual days, helping patients see that a difficult day doesn't ruin a week and that consistency matters more than perfection. The data belongs to them, and the relationship with that data should feel supportive rather than surveilling. If checking the dashboard becomes stressful, we'll discuss that, because the goal is building appetite literacy and self-trust, not creating a new form of food obsession that happens to have my clinic's name on it.
What the care team will see
What makes this different from tracking alone is the relationship that surrounds it, because data without interpretation just becomes another source of anxiety. Your care team will see the same dashboard you see, which means we can notice patterns together. Maybe your protein drops on weekends when your routine changes and you're eating whatever the kids want, or maybe your hydration suffers during particularly stressful weeks at work when you forget to drink anything except coffee until 3 PM. Maybe your evening eating tends to spike on days when you skip breakfast entirely, which tells us something important about how the structure of your day affects what happens at night.
I've already been observing these patterns through RxFood for a few years. The Nourish Score provides a shared language for discussing them, a way to discuss nutrition that focuses on the components that actually matter for appetite regulation rather than getting lost in calorie counts or macronutrient percentages that obscure more than they reveal. When I tell a patient, "I'm noticing that your scores drop on the days when you have back-to-back meetings through lunch," she has a specific consideration and experiment to consider and experiment with. Maybe she needs to block fifteen minutes before noon as protected eating time. Maybe she needs protein-dense snacks in her desk drawer for the days when lunch genuinely isn't possible. Perhaps we need to discuss whether her calendar reflects her values or simply accommodates others' demands at the expense of her own basic needs.
The interpretation happens in relationship, which is what transforms raw numbers into useful insight. A low score in isolation tells you nothing about why it happened or what to do differently. A low score in conversation with a care team that knows your history, your challenges, and your particular Tuesday chaos becomes the starting point for figuring out what would actually help. That conversation is where the real work happens, and the dashboard exists to support it.
Feeding yourself with care
Most of my patients have spent years, sometimes decades, caring for everyone else with tremendous skill and attention. They know their children's allergies, their partner's dietary preferences, and their aging parents' medication regimens. They track appointments and deadlines and needs that belong to other people with remarkable competence, while their own needs get pushed to the margins. When I ask them what they ate yesterday, many of them go blank, and when I ask whether they're getting enough protein, they have no idea. When I ask when they last felt genuinely satisfied after a meal, satisfied without being uncomfortably full, satisfied without guilt, just satisfied, they often can't remember because that experience has become so rare.
This disconnection from their own eating reflects years of training the nervous system to prioritize others' needs over one's own, and it manifests in the body as a loss of connection to basic signals. The hunger and fullness cues never stopped arriving, but the constant noise of others' demands made those signals easy to ignore until ignoring them became automatic, which is why so many women describe feeling completely out of touch with their own appetite by the time they reach midlife. Reconnecting with those signals requires attention, practice, and permission. Permission to notice what you need. Permission to respond to that noticing by actually eating. Permission to feed yourself with the same care you've always extended to everyone else in your life.
The Nourish Score serves the larger purpose of reconnection by making tracking what you eat a way of paying attention to yourself, which many accomplished women rarely experience as adults. The score provides structure for that attention, a framework that helps you notice patterns you couldn't see when eating felt chaotic and overwhelming, and the days blurred together without a clear memory of what went where. Over time, as you begin to understand which eating patterns leave you feeling regulated, and which ones don't, you need the structure less because you've internalized the skill of reading your own experience, and the dashboard becomes a check-in rather than a crutch.
What medication makes possible
If you're taking a GLP-1 medication or considering one, everything I've described becomes more urgent rather than less. Medication creates space by quieting the constant food noise that has dominated your mental landscape for years, and for many patients, this represents the first time they can remember going whole afternoons without thinking about food, without feeling hijacked by cravings, without battling their own appetite just to get through the day. That clarity is the benefit that medication offers, and it's genuinely transformative for people who have unsuccessfully fought their biology for decades.
The question becomes what you do with that space, because the space itself teaches you nothing about how to eat well. Without attention to protein, you risk losing muscle mass alongside fat, which tanks your metabolism and creates conditions for regain down the line even if you stay on medication indefinitely. Without fibre, the gut changes that support lasting appetite regulation don't happen, which means you remain dependent on the medication to do work that your body could eventually do on its own with proper support. Without understanding how timing affects your metabolic function, you might interpret the reduced appetite as permission to skip meals entirely, leading to under-eating patterns that accelerate muscle loss and leave you feeling depleted even as the scale moves in the direction you wanted.
I've watched this play out dozens of times through the nutrition data in RxFood: patients whose caloric intake drops to 600 or 800 calories per day without them realizing it, patients whose protein intake collapses because the foods they used to enjoy now trigger nausea, patients who need dose adjustments that nobody catches because nobody is watching their nutrition closely enough. The Nourish Score is designed to make these patterns visible early, before suffering accumulates, before side effects drive medication discontinuation, and before metabolic damage becomes difficult to reverse.
Patients who thrive on medication use the space it creates to finally nourish themselves properly, eating enough protein to protect their muscle mass, enough fibre to support their gut health, and enough food overall to fuel their lives. They pay attention to what they're eating, track their patterns, notice what works, and build eating habits that will support them regardless of what happens with medication in the future. Medication without education produces weight loss that remains fragile because it depends entirely on the continued presence of the drug rather than on skills and understanding that belong to the patient herself.
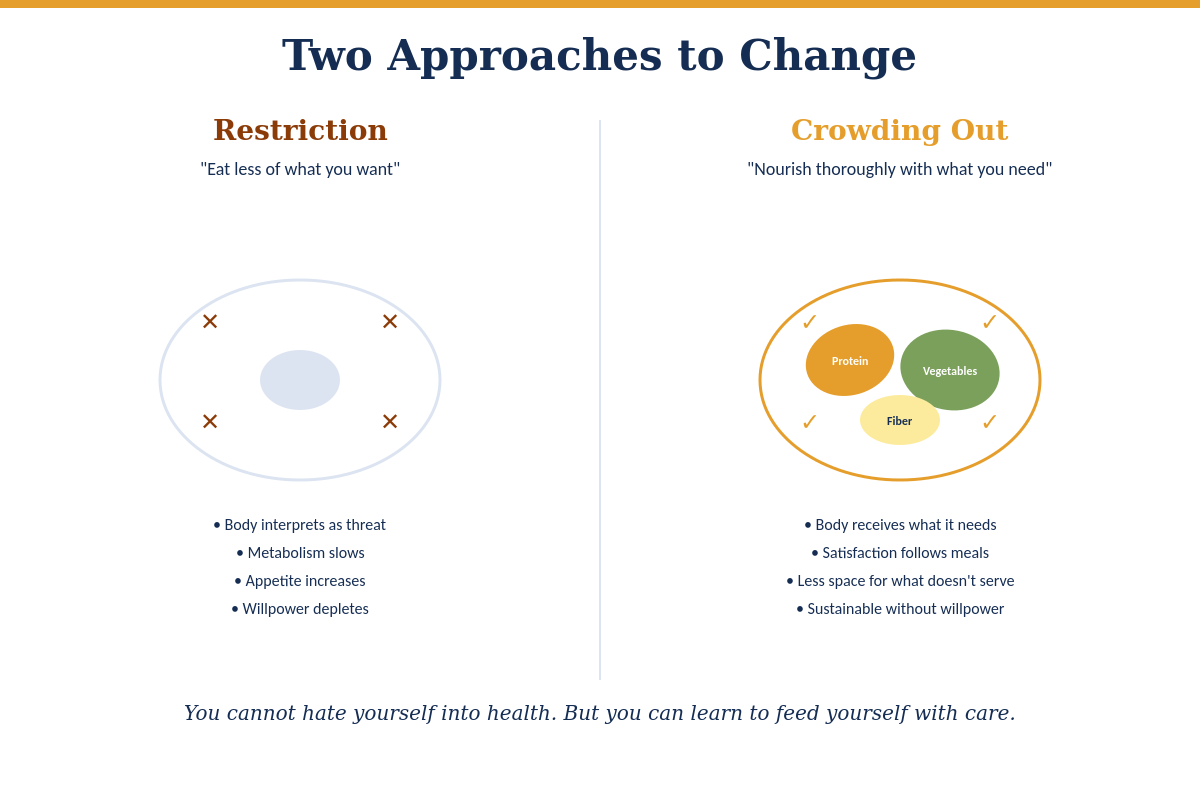
Crowding out
At The Shift, we talk about crowding out as the operating principle behind how we think about nutrition, because restriction fails for biological reasons having nothing to do with character or commitment. When you restrict your eating, your body interprets the reduction as a threat and responds accordingly. Metabolism slows to conserve energy. Appetite hormones shift to drive eating. The very systems designed to keep you alive begin working against your stated goals with remarkable persistence. You can fight this response temporarily through force of will, but the body eventually wins because it's designed to win these battles, which is why every diet you've abandoned and every plan you've "fallen off" represents your survival systems doing exactly what evolution built them to do.
Crowding out is straightforward: nourish yourself well and regularly with what your body actually needs, so that there's naturally less space for what doesn't serve you, which means you're adding rather than subtracting. When you prioritize enough food at breakfast, you don't need to ban carbohydrates or swear off the foods you enjoy; you simply find yourself satisfied through your 10 AM meeting in a way that makes the vending machine less compelling because you're genuinely not hungry. When you fill half your plate with vegetables, you're leaving less room for options that would leave you hungry again in an hour, and the math of your plate shifts without requiring deprivation or heroic self-denial.
This approach changes your relationship with food from adversarial to supportive. Food becomes something that helps you feel good rather than something you have to control and constantly resist. You can eat with enjoyment and attention rather than guilt and calculation. The Nourish Score supports this reframe by measuring how well you're feeding yourself rather than how effectively you're depriving yourself, which leads to different outcomes because it orients you toward a different goal entirely.
What becomes possible
I built the Shift Nourish Score because I've spent years watching women struggle with nutrition tools that weren't designed for them, and I wanted something better. I wanted a score that measures what actually matters for appetite regulation. I wanted a dashboard that informs without shaming. I wanted a framework that supports the larger work of reconnecting with your body rather than creating another source of anxiety about food.
This week, that tool becomes real. It joins the larger framework of comprehensive care at The Shift Clinic, which includes medical treatment, appetite literacy development, community support, and ongoing access to a care team that knows your history, your challenges, and your particular Tuesday chaos. The nutrition piece matters, but it only works when it's integrated into something larger, held within relationships that see you as a whole person rather than a collection of macros to optimize.
If you've been collecting nutrition data for years without feeling any closer to understanding your own body, the problem might be that you need different information, interpreted within a relationship that supports your growth rather than your compliance. That's what comprehensive weight care actually looks like: a relationship that helps you become the person who knows how to feed herself well, not because she memorized the rules, but because she finally learned to pay attention.
Ready to see what this looks like in practice?Start here.